A Conservative Restorative Approach for a Patient With Cleft Palate: Replacing a Lateral Incisor and Enhancing Esthetics
Abstract: Young patients often times are poor candidates for implant-supported restorations due to ongoing jawbone development. This case report describes a viable restorative option for a 16-year- old patient who had a large cleft defect and a hopeless prognosis for the right lateral incisor. The clinician utilized a combination of a fixed bonded ceramic restoration to replace tooth No. 7 and direct composite resin, including pink composite resin, to restore the symmetry and gingival level of tooth No. 8. This conservative approach allowed for an esthetic outcome while providing the patient a stable and functional restoration.
Advances in ceramic systems, adhesive resin cements, and computer-aided design/ computer-assisted manufacturing (CAD/ CAM) technology have expanded the range of conservative treatment options available for fixed prosthetic rehabilitation. These innovations enhance the quality, esthetics, and predictability of dental care, provid- ing effective solutions for complex restorative cases, particu larly when replacing missing anterior teeth.
Case Report
A 16-year-old female patient was referred by her orthodon tist for evaluation and restorative treatment following eleft palate surgery and orthodontic therapy. The patient was in good general health, and her present medical history was noncontributory. The patient was adopted from China at 2 years of age. She was evaluated by the cleft and craniofacial team at Wake Forest University with a diagnosis of right unilateral cleft lip and alveolus, submucous cleft palate, and a deficient soft palate, resulting in hypernasal speech.
Medical and Surgical History: The patient had under- gone multiple surgical procedures, including initial cleft lip repair in China prior to adoption, pharyngeal flap for velo- pharyngeal insufficiency (VPI) at 3 years old, cleft lip revi- sion at 4 years old, and an alveolar bone graft at 8 years old.
Orthodontic History: The patient initially presented to the orthodontist at age 13 years, with no prior orthodontic treatment, and was diagnosed with the following; class 1 malocclusion, no posterior crosshite present, and accept able anterior-posterior skeletal relationship and overbite.

Fig 1. Preoperative extraoral view of the patient with lips at rest. Fig 2. Preoperative extraoral view of the patient smil Ing. Fig 3. Radiograph revealed substantial bone loss surrounding tooth No. 7 and a visible cleft defect between teeth Nos. 7 and 8
The maxillary midline was positioned to the right of the Facial midline. The maxillary right cuspid occupied the maxillary right lateral space, with a poorly formed maxil- Jary right lateral incisor lingual to the right cuspid. The prognosis for the maxillary right lateral incisor was poor However, preservation of this tooth initially was consid- ered important to prevent alveolar bone loss. It is typi cal for cleft lip and palate patients to exhibit significant defects in soft tissue, alveolar bone, and tooth anomalies. in the cleft site. Orthodontic treatment was completed in 2 years and referred for comprehensive periodontal/pros- thetic rehabilitation after placing into retention.
At the time of her visit with the restorative dentist, the patient’s primary concern was, “I would like to fix my smile.” A clinical extraoral evaluation revealed a deviated facial midline and a slanted incisal plane, with a normal maxillary incisal display at rest (Figure 1 and Figure 2).
Intraoral and radiographic evaluation indicated that tooth No. 7 had a hopeless prognosis due to significant bone loss, an unfavorable crown-to-root ratio, mobility, malposition, a short conical root, and a peg lateral shape (Figure 3). Additionally, there was a large cleft defect between teeth Nos. 7 and 8. From an esthetic perspec tive, the central and lateral incisors were asymmetrical, with significant gingival recession and an irregular gingival outline between teeth Nos. 7 and 8 (Figure 4). A noticeable midline cant leaning toward the patient’s left side could not be corrected orthodontically due to the root position of tooth No. 8, which would have moved into the cleft defect (Figure 2).
Given the patient’s young age, esthetic concerns, and biological considerations, a ceramic resin-bonded fixed dental prosthesis (RBFDP) was recommended to replace tooth No. 7, and a direct bonded restoration using the injectable technique was planned for tooth No. 8 to create symmetry and improve the midline cant, enhancing the esthetic appearance. Additionally, a diagnostic occlusal splint was recommended to protect the new restorations.
Esthetic Analysis
The treatment planning began with an esthetic evalua- tion, followed by considerations of function, structure, and biology. A seven-step esthetic analysis, as described by Chiche, was conducted to detect potential “esthetic red flags” early in the planning stage. The first four steps of the analysis focused on evaluating the incisal edge position of the maxillary central and lateral incisors, which form the foundation for an optimal smile. This evaluation was facili- tated through a digital wax-up design, printed diagnostic casts, and a smile trial to determine the appropriate tooth proportions and gingival levels (Figure 5 and Figure 6).
Extraction of Tooth No. 7; Direct Bonded Restoration of Tooth No. 8
As planned, tooth No. 7 was extracted (Figure 7), and a direct injectable composite restoration was performed on tooth No. 8. A clear silicone matrix (Memosil 2, Kulzer, kulzer.com) was fabricated from the 3D-printed
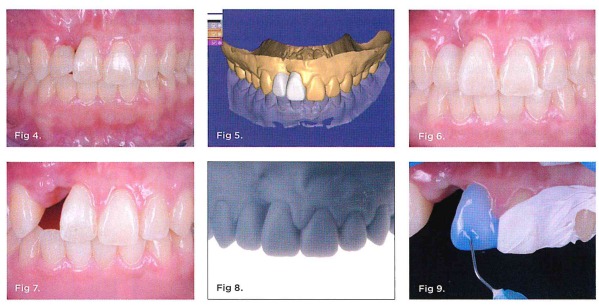
Fig 4. Preoperative intraoral view showing an irregular gingival contour, absence of papillae between teeth Nos. 7 and 8, and gingival recession. Fig 5. Digital diagnostic wax-up. Fig 6. Smile trial. Fig 7. Post-extraction of right lateral incisor Fig 8. 3D-printed diagnostic wax-up cast. Fig 9. cast. Fig 9. Etching with 35% phosphoric acid after tooth No 8 was cleaned and rinsed.
diagnostic wax-up cast used for the mock-up (Figure 8). Tooth No. 8 was cleaned with pumice and rinsed. A tooth cleaner (Katana™ Cleaner, Kuraray, kuraraydental.com) was applied to the surface of tooth No. 8 for 20 seconds and then rinsed off with water. The enamel was etched with 35% phosphoric acid (K-Etchant Syringe, Kuraray) for 15 seconds and rinsed (Figure 9). A triple-zero cord (Ultrapak Cord, Ultradent, ultradent.com) was placed to protect the sulcus, and bonding adhesive (Clearfil Universal Bond Quick, Kuraray) was applied and light- cured (Figure 10). The clear silicone matrix was seated, and flowable composite shade A2 (Clearfil Majesty ES Flow, Kuraray) was injected into the matrix through a 1-mm access hole (Figure 11 and Figure 12). After removal of the matrix, the composite was polished and finished with diamond dises (Figure 13).7
Preparation and Delivery of RBFDP; Direct Pink Composite Resin on Tooth No. 8
A conservative intra-enamel preparation was performed on the lingual aspect of abutment tooth No. 6 to support the RBFDP (Figure 14). A single zirconia cantilever retainer prosthesis with a facial cutback design was selected for this case to benefit from the strength of the zirconia substructure (Katana™ Zirconia HTML, Kuraray) and the esthetic, natural appearance of layered feldspathic porce- lain (Cerabien™ ZR [CZR] porcelain, Kuraray) (Figure 15 through Figure 18).
The single-retainer RBFDP utilizing zirconia as the substructure ceramic system offers excellent long-term
success and is a conservative option for patients who are not candidates for implant restoration due to age, poor bone quantity or quality, or root position of adjacent teeth.”
To maximize the bond strength of the restoration, the prosthesis was pretreated in the laboratory before cemen- tation. The adhesive surface of the zirconia was treated with airborne particle abrasion using 50-µm aluminum oxide particles at 2.5 bar pressure. A ceramic primer (Clearfil Ceramic Primer Plus, Kuraray) was applied.2.10 The abutment tooth was prepared as follows: it was cleaned with pumice and Katana Cleaner, etched with 35% phos- phoric acid for 40 seconds, and adhesive was applied but not cured. A dual-cure resin cement (Panavia™ SA Cement Universal, Kuraray) was applied to the intaglio surface of the prosthesis and seated. The cement was initially light- cured for 4 seconds while the prosthesis was held in posi- tion. Excess cement was then removed, and final curing was completed. The recession on tooth No. 8 was restored using pink composite (Gradia, GC America, gc.dental/ america) (Figure 19 and Figure 20).
Conclusion
The described procedure is a viable option for young patients missing a lateral incisor who are not candidates for implant-supported restorations. In this case, due to the large soft-tissue defect between teeth Nos. 7 and 8, a combination of a fixed bonded ceramic restoration to replace tooth No. 7 and direct composite resin, including pink composite resin, to restore the symmetry and gingival level of tooth No. 8 was utilized. By using a conservative approach, the dental team was able to achieve the esthetic outcome desired by the patient while providing a stable and functional restoration.
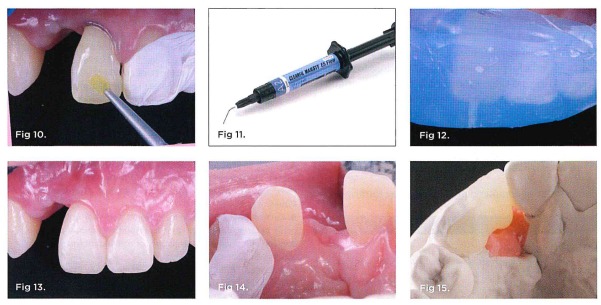
Fig 10. Following retraction cord placement, adhesive bonding was applied. Fig 11. Flowable composite shade A2. Fig 12. Injection of the flowable composite resin. Fig 13. Composite restoration completed. Fig 14. Lingual view of the canine after intra-enamel preparation. Fig 15. Following CAD/CAM design of the zirconia substructure, this photograph shows a lingual view of the restoration on the working cast
ACKNOWLEDGMENT
The authors thank Jeff Ganeles, DMD, periodontist in Boca Raton, Florida, for his invaluable contributions to this case. They also extend their appreciation to master ceramists Anastasiia Melnyk and Samuel Madera for their exceptional craftsmanship and expertise in achieving the final esthetic and functional outcomes.
ABOUT THE AUTHORS
Sergio R. Arias, DDS, MS
Private Practice limited to Prosthodontics and Esthetic Dentistry, Fort Lauderdale, Florida
Barry I. Malza, DMD
Lead orthodontist for the craniofacial team at Joe DiMaggio Children’s Hospital, Hollywood, Florida; Private Practice limited to Orthodontics, Boca Raton, Florida
